Shoulder arthrosisIs chronic a disease in which the tissue of the articular cartilage is destroyed and thinned, pathological changes in soft tissues occur, and bone growths are formed in the area of the joint. It is manifested by pain and crunching in the affected area. In the later stages, the range of motion decreases. Pathology is chronic and gradually progresses. The diagnosis is made taking into account the clinical picture and radiological signs. Treatment is usually conservative: physiotherapy, anti-inflammatory drugs, chondroprotectors, exercise therapy. When the joint is destroyed, arthroplasty is performed.
a disease in which the tissue of the articular cartilage is destroyed and thinned, pathological changes in soft tissues occur, and bone growths are formed in the area of the joint. It is manifested by pain and crunching in the affected area. In the later stages, the range of motion decreases. Pathology is chronic and gradually progresses. The diagnosis is made taking into account the clinical picture and radiological signs. Treatment is usually conservative: physiotherapy, anti-inflammatory drugs, chondroprotectors, exercise therapy. When the joint is destroyed, arthroplasty is performed.
General information
Arthrosis of the shoulder joint is a chronic disease in which, as a result of degenerative-dystrophic processes, the cartilage and other tissues of the joint are gradually destroyed. Usually arthrosis affects people 45 years and older, but in some cases (after injury, inflammation), the disease may develop at a younger age. Pathology equally often occurs in women and in men, more often observed in athletes and in people engaged in hard physical labor.
The reasons
The starting point for changes in arthrosis of the shoulder joint can be both the normal aging process of tissues and damage or disruption of the cartilage structure as a result of mechanical influences and various pathological processes. Primary arthrosis is usually detected in the elderly, secondary (developed against the background of other diseases) can occur at any age. The main reasons are considered:
- Developmental defects.Pathology can be detected with underdevelopment of the head of the humerus or glenoid cavity, shoulder capomelia and other anomalies of the upper limb.
- Traumatic injury.Arthrosis of traumatic etiology most often occurs after intra-articular fractures. A possible cause of the disease can be a dislocation of the shoulder, especially the usual one. Less often, severe bruises act as a provoking injury.
- Inflammatory processes.The disease can be diagnosed with long-term shoulder-scapular periarthritis, previously suffered nonspecific purulent arthritis and specific arthritis of the joint (with tuberculosis, syphilis and some other diseases).
Risk factors
Arthrosis is a polyetiological disease. There is a wide group of factors that increase the likelihood of this pathology:
- Hereditary predisposition.Many patients have close relatives who also suffer from arthrosis, including those of other localizations (gonarthrosis, coxarthrosis, arthrosis of the ankle joint).
- Overstrain of the joint.It can occur in volleyball players, tennis players, basketball players, throwers of sports equipment, as well as in people whose profession involves a constant high load on their hands (hammers, loaders).
- Other pathologies. Arthrosis is more often detected in patients suffering from autoimmune (rheumatoid arthritis), some endocrine diseases and metabolic disorders, systemic connective tissue insufficiency and excessive joint mobility.
The likelihood of developing the disease increases dramatically with age. Frequent hypothermia and unfavorable environmental conditions have a certain negative impact.
Pathogenesis
The main reason for the development of arthrosis of the shoulder joint is a change in the structure of the articular cartilage. The cartilage loses its smoothness and elasticity, the sliding of the articular surfaces during movement becomes difficult. Microtrauma occurs, which lead to further deterioration of the condition of the cartilage tissue. Small pieces of cartilage "break off" from the surface, forming free-lying articular bodies, which also injure the inner surface of the joint.
Over time, the capsule and synovium thicken, areas of fibrous degeneration appear in them. Due to thinning and a decrease in elasticity, the cartilage ceases to provide the necessary shock absorption, therefore, the load on the underlying bone increases. The bone deforms and grows along the edges. The normal configuration of the joint is disrupted, there are limitations of movement.
Classification
In traumatology and orthopedics, a three-stage systematization is usually used, reflecting the severity of pathological changes and symptoms of arthrosis of the shoulder joint. This approach allows you to choose the optimal medical tactics, taking into account the severity of the process. The following stages are distinguished:
- The first- there are no gross changes in the cartilage tissue. The composition of the synovial fluid is changed, the nutrition of the cartilage is impaired. Cartilage does not tolerate stress, therefore, joint pain (arthralgia) occurs from time to time.
- The second- the cartilage tissue begins to thin, its structure changes, the surface loses its smoothness, cysts and areas of calcification appear in the depths of the cartilage. The underlying bone is slightly deformed, bone growths appear along the edges of the articular platform. The pains become permanent.
- Third- marked thinning and disruption of the cartilage structure with extensive areas of destruction. The articular platform is deformed. Revealed limitation of range of motion, weakness of the ligamentous apparatus and atrophy of the periarticular muscles.
Symptoms
In the early stages, patients with arthrosis are concerned about discomfort or slight pain in the shoulder joint during exertion and certain body positions. Crunching may occur during movement. The joint is not externally changed, there is no edema. Then the intensity of pain increases, arthralgias become habitual, constant, appear not only during exercise, but also at rest, including at night. Distinctive features of pain syndrome:
- Many patients note the dependence of the pain syndrome on weather conditions.
- Along with aching pain, over time, there is a sharp soreness during physical exertion.
- Pain can occur only in the shoulder joint, radiate to the elbow joint, or spread throughout the arm. Possible back and neck pain on the affected side.
After a while, patients begin to notice a noticeable morning stiffness in the joint. The range of motion decreases. After exercise or hypothermia, slight swelling of soft tissues is possible. With the progression of arthrosis, movements are more and more limited, contractures develop, and the function of the limb is seriously impaired.
Diagnostics
The diagnosis is made by an orthopedic surgeon taking into account the characteristic clinical and radiological signs of arthrosis of the shoulder joint. If you suspect secondary arthrosis, consult a surgeon, endocrinologist. The joint is initially not changed, later it is sometimes deformed or enlarged. On palpation, pain is determined. Restriction of movement may be detected. To confirm arthrosis, the following are recommended:
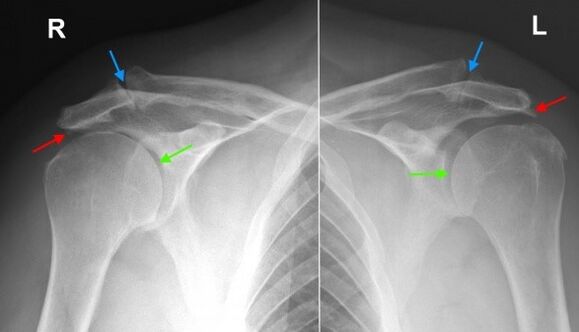
- Radiography of the shoulder joint.Dystrophic changes and marginal bone growths (osteophytes) are found, in the later stages narrowing of the joint space, deformation and changes in the structure of the underlying bone are determined. The joint gap can acquire a wedge-shaped shape, osteosclerotic changes and cystic formations are visible in the bone.
- Tomographic research. In doubtful cases, especially in the initial stages of the disease, CT of the shoulder joint is performed to obtain additional data on the condition of the bone and cartilage. If it is necessary to assess the condition of soft tissues, magnetic resonance imaging is performed.
Differential diagnosis
The differential diagnosis of arthrosis is carried out with gouty, psoriatic, rheumatoid and reactive arthritis, as well as with pyrophosphate arthropathy. With arthritis, a blood test shows signs of inflammation; changes on radiographs are not very pronounced, osteophytes are absent, there are no signs of deformation of the articular surfaces.
In psoriatic arthritis, along with articular manifestations, skin rashes are often found. In rheumatoid arthritis, a positive rheumatoid factor is determined. In case of pyrophosphate arthropathy and gouty arthritis, the biochemical blood test reveals corresponding changes (an increase in the level of uric acid salts, etc. ).
Shoulder arthrosis treatment
Patients are under the supervision of an orthopedic surgeon. It is necessary to limit the load on the arm, excluding sudden movements, lifting and prolonged carrying of weights. At the same time, it should be borne in mind that inaction also negatively affects the diseased joint. To maintain the muscles in a normal state, as well as to restore the shoulder joint, you need to regularly perform the exercise therapy complex recommended by the doctor.
Conservative treatment
One of the most urgent tasks in arthrosis is the fight against pain. To eliminate pain and reduce inflammation, the following are prescribed:
- General action drugs.NSAIDs are prescribed in tablets during an exacerbation. With uncontrolled use, they can irritate the wall of the stomach, have a negative effect on the state of the liver and metabolism in the cartilaginous tissue, therefore, they are taken only as directed by a doctor.
- Local remedies.NSAIDs are commonly used in the form of gels and ointments. Self-administration is possible if symptoms arise or intensify. Less commonly, topical hormone preparations are indicated, which should be applied in accordance with the doctor's recommendations.
- Hormones for intra-articular administration.In case of severe pain syndrome, which cannot be eliminated by other methods, intra-articular administration of drugs (triamcinolone, hydrocortisone, etc. ) is performed. Blockades are carried out no more than 4 times a year.
To restore and strengthen cartilage at stages 1 and 2 of arthrosis, agents from the group of chondroprotectors are used - drugs containing hyaluronic acid, chondroitin sulfate and glucosamine. The courses of treatment are long (from 6 months to a year or more), the effect becomes noticeable after 3 or more months.
Physiotherapy treatment
For arthrosis of the shoulder joint, massage, physiotherapy exercises and physiotherapy techniques are actively used. During the period of remission, patients are referred for spa treatment. Apply:
- mud therapy and paraffin;
- medicinal baths;
- magnetotherapy and infrared laser therapy;
- ultrasound.
Surgery
At stage 3 of the disease, with significant destruction of cartilage, limitation of mobility and disability, arthroplasty of the joint is performed. The referral for the operation is given taking into account the patient's age, the level of his activity, the presence of severe chronic diseases. The use of modern ceramic, plastic and metal endoprostheses allows you to fully restore the function of the joint. The service life of prostheses is 15 years or more.
Forecast
Arthrosis is a long-term, gradually progressive disease. It cannot be completely cured, however, it is possible to significantly slow down the development of pathological changes in the joint, to preserve the ability to work and a high quality of life. To achieve the maximum effect, the patient must take a serious attitude towards his illness and his readiness to follow the doctor's recommendations even during the period of remission.
Prophylaxis
Preventive measures include reducing domestic injuries, observing safety at work, eliminating excessive loads on the shoulder joint when performing professional duties and playing sports. It is necessary to timely diagnose and treat pathologies that can provoke the development of arthritic changes.



































